Haga clic aquí para ver esta página web en español.
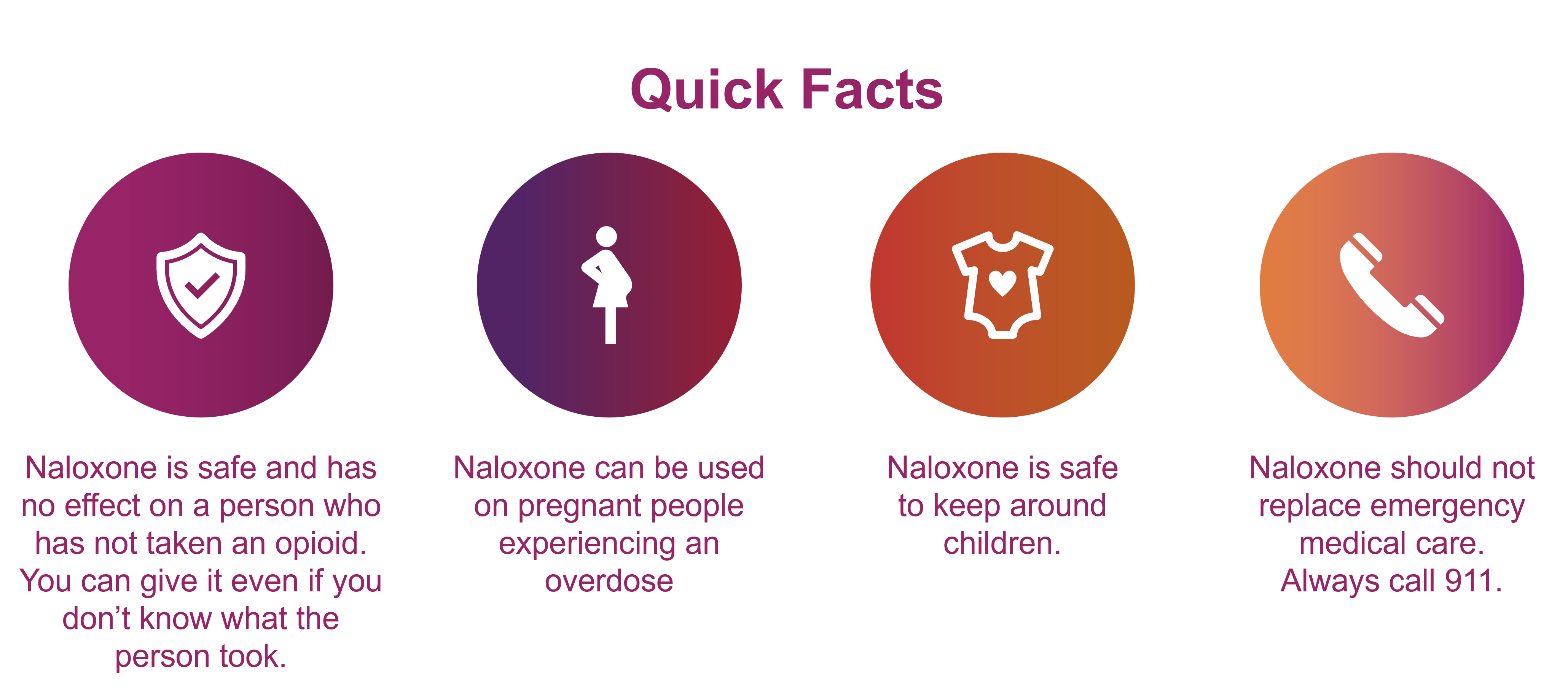
Anyone—including you—can give naloxone to someone who is experiencing an overdose.
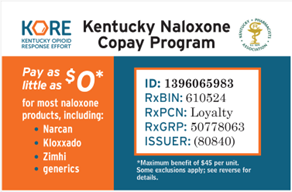
Naloxone (also known as the brand names Kloxxado™, Narcan®, RiVive™, or Zimhi®) is a medicine that can save someone’s life if they overdose on opioids—whether it’s a prescription opioid, heroin, or an illicit drug containing fentanyl. Naloxone quickly blocks and reverses the effects of an opioid overdose. You can tell it is working because it quickly helps a person breathe normally. It is not a treatment for opioid use disorder (OUD) or opioid misuse.
Naloxone nasal spray is a ready-to-use medicine that can be given without any special training. The spray bottle is small and can fit in your pocket, purse, or glove compartment.
Carrying naloxone does not mean that you are encouraging people to misuse opioids or other drugs. It just means that you are ready to save a life in an emergency.